This article was analyzed by Serge, MSc. Leveraging expertise in Biochemistry and Chemical Quality Control, I share insights and recommendations backed by research and clinical evidence to ensure you find safe and effective supplement solutions.

For decades, Parkinson’s disease has been seen as a brain-first disorder, a neurological condition that damages the brain’s dopamine-producing cells, causing the classic tremors, stiffness, and slowed movement we associate with the disease. But a groundbreaking new study published in Nature Neuroscience in 2025 challenges that core assumption.
Led by researchers at Wuhan University in China, the study presents compelling evidence that Parkinson’s may actually originate in the kidneys, a surprising and potentially game-changing insight into one of the world’s most complex neurodegenerative diseases.

A- Parkinson’s Disease: A Quick Overview.
Parkinson’s disease (PD) affects more than 10 million people worldwide, primarily striking individuals over the age of 60. It’s known for damaging neurons in the brain, especially in a region called the substantia nigra, leading to **a sharp decline in dopamine, the chemical messenger responsible for smooth, coordinated movement.
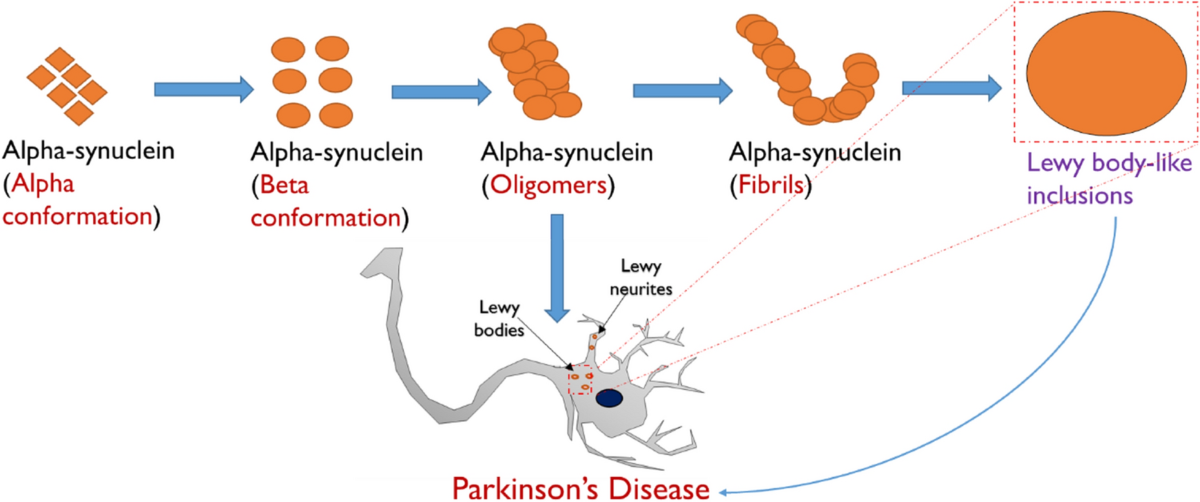
A key player in Parkinson’s pathology is a protein called alpha-synuclein (α-Syn). When α-Syn misfolds and clumps together in the brain, it forms what are known as Lewy bodies, toxic buildups that interfere with brain function and accelerate neurodegeneration.
B-The New Discovery: Kidney Connection.
The new study focused on where those damaging α-Syn clumps might actually begin.
The surprising finding? The kidneys appear to be a significant early site for abnormal α-Syn buildup, even before any signs of brain damage.
> “We demonstrate that the kidney is a peripheral organ that serves as an origin of pathological α-Syn,” write the researchers in their published paper.
To reach this conclusion, the team conducted a multi-layered investigation, including:
-Genetically engineered mouse models.
-Human tissue samples from individuals with Parkinson’s, dementia, and chronic kidney disease (CKD).
C- Key Findings from the Study.
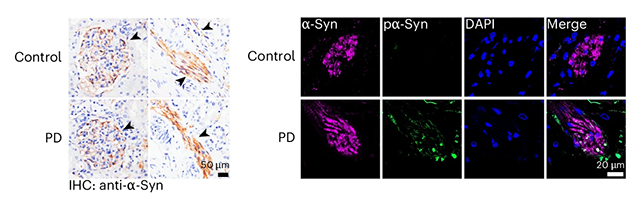
1. α-Syn Found in the Kidneys of Parkinson’s Patients.
In tissue samples from 11 human subjects with Parkinson’s or dementia with Lewy bodies, 10 showed α-Syn clumps in the kidneys.
This suggests α-Syn may accumulate in peripheral organs before traveling to the brain.
2. Kidney Disease May Precede Neurological Symptoms.
In a separate group of 20 patients with chronic kidney disease but no neurological issues, 17 had abnormal α-Syn levels in their kidneys.
This is a strong indicator that kidney dysfunction might trigger or worsen Parkinson’s, rather than being a side effect.
3. Mouse Models Confirm the Spread.
In healthy mice, the kidneys were able to clear the injected α-Syn proteins from their system. However, in mice with kidney dysfunction, these proteins built up over time and eventually traveled to the brain, causing damage.
What’s even more interesting is that when researchers cut the nerves connecting the brain and kidneys, the spread of the α-Syn proteins stopped, suggesting a direct link between the kidneys and the brain in the progression of the disease.
4. Blood Plays a Role Too.
Researchers also found that reducing α-Syn levels in the blood led to less damage in the brain.
This suggests a promising new direction for treatment: using blood-based therapies to stop the disease from reaching the brain in the first place.
D- Limitations of the Study.
While this discovery is exciting, there are a few important limitations to keep in mind:
-
The number of human samples in the study was small, so larger studies are needed to confirm the findings.
-
Although mice are commonly used in research, they don’t perfectly represent how the human body works, so further testing in humans is essential.
-
And finally, just finding α-Syn in the kidneys doesn’t prove it causes Parkinson’s, but it does make the connection worth exploring further.
E- Why This Matters: A New Frontier in Parkinson’s Research.
Parkinson’s is a complex disease, and scientists have long believed it has multiple triggers. One possible starting point is the gut, another organ outside the brain where α-Syn buildup has been found. This new study adds the kidneys to that list, challenging how we understand the origins of neurodegenerative diseases.
The potential implications are huge:
-
Early detection: If we can measure α-Syn buildup in the kidneys, it might be possible to diagnose Parkinson’s years before symptoms appear.
-
New treatment options: Therapies aimed at the kidneys or bloodstream could help slow or even stop the disease’s progression.
-
A holistic approach: This research supports a shift away from thinking of Parkinson’s as just a brain disease, instead, it highlights the importance of whole-body health in neurodegeneration.
F- What’s Next?
Future research will likely focus on:
-Validating these findings** with larger human studies.
-Developing diagnostics** that measure α-Syn levels in the kidneys or blood.
-Creating new treatments** that focus on clearing α-Syn from the body, not just the brain.
As the researchers note in the paper:
“Removal of α-Syn from the blood may hinder the progression of Parkinson’s disease, providing new strategies for therapeutic management of Lewy body diseases.”
G- Final Thoughts.
This study could change the way we think about Parkinson’s disease. While more research is needed, the idea that Parkinson’s might start outside the brain, in the kidneys or other parts of the body, could lead to new ways to find, treat, and maybe even prevent the disease.
One thing is clear: fighting Parkinson’s is not just about the brain anymore. It’s a whole-body challenge, and this new research gives us another important clue to help solve it.
Study reference: Yuan et al., “Peripheral α-Synuclein Accumulation in the Kidneys as a Potential Trigger for Parkinson’s Disease,” Nature Neuroscience, 2025.